Dentists exempted from Maine’s COVID-19 vaccine mandate
The final version of Maine’s COVID-19 vaccination mandate does not include dentists or emergency medical service workers, the Portland Press-Herald reported. Dental health facilities were exempted because of an absence of COVID-19 outbreaks. “Maine dentists have high vaccination rates and have taken many steps to help prevent the spread of COVID-19 in their offices,” said Kathy Ridley, the Maine Dental Association’s interim executive director. “There have been no identified COVID-19 outbreaks originating from a dental health practice in Maine.”
Full Story: SmartBrief – Industry E-mail Newsletters for Professionals
Portland Press Herald (Maine) (tiered subscription model) (11/11)
Dental News
PA’s oldest working dentist is in no hurry to retire
Ike Roepcke, D.D.S., at age 94, is the oldest working dentist in Pennsylvania, according to the Pennsylvania Dental Association, and while he stopped seeing patients last year due to the COVID-19 pandemic, he continues to work making dentures for his son’s practice in Langhorne. “I won’t stop working, and I’ll tell you why,” Dr. Roepcke told the Bucks County Courier Times. “We men don’t do well if we’re just sitting around with not much to do. We don’t last long. I’ve seen it over and over. So don’t retire.” Dr. Roepcke’s family left Germany for America in the 1930s and he enlisted in the US Navy in 1944 at age 17, but before he could see active duty, World War II ended. A Navy dentist suggested he try dentistry as a profession so he enrolled in the University of Pennsylvania dental school. Dr. Roepcke opened his first dental office in Bristol, Pa., later moving it to a home he built in Langhorne.
Full Story: http://r.smartbrief.com/resp/oqphCJwxjADqwluWCifOisBWcNsigw?format=multipart Bucks County Courier Times (Levittown, Pa.) (9/21)
Tooth Loss Linked With Increased Risks of Cognitive Impairment and Dementia
According to researchers at Rory Meyers College of Nursing, tooth loss is a risk factor for cognitive impairment and dementia. Researches also found that the risk is not significant among older adults with dentures. According to a study, adults with more tooth loss had a 1.48 times higher risk of developing cognitive impairment and 1.28 times higher risk of being diagnosed with dementia. “Given the staggering number of people diagnosed with Alzheimer’s disease and dementia each year, and the opportunity to improve oral health across the lifespan, it’s important to gain a deeper understanding of the connection between poor oral health and cognitive decline,” said senior author Bei Wu, PhD, Dean’s Professor in Global Health at the NYU Rory Meyers College of Nursing and codirector of the NYU Aging Incubator. “Our findings underscore the importance of maintaining good oral health and its role in helping to preserve cognitive function,” said Wu.
Full Story: https://www.dentistrytoday.com/tooth-loss-linked-with-increased-risks-of-cognitive-impairment-and-dementia/
JADA study: COVID-19 incidence lower among dentists than other health care workers
A study reported in the Journal of the American Dental Association found that dentists had experienced a 2.6% cumulative COVID-19 infection rate as of November 2020, with monthly incidence rates ranging from 0.2% to 1.1% and averaging 0.5% over six months. This infection rate is far below that of other health care workers, such as physicians and nurses, ADA News reports.
“We’re pleased to see that dentists have demonstrated continued low monthly incidence of disease despite several regional and national COVID-19 rate spikes during the study period,” said Marcelo Araujo, D.D.S., Ph.D., CEO of the ADA Science & Research Institute, chief science officer of the ADA and senior author of the report. “This study shows high rates of pre-appointment screening of patients and appropriate infection control measures throughout the study period, demonstrating that adhering to very strict protocols for enhanced infection control helps protect their patients, their dental team and themselves,” Dr. Araujo said.
Full Story: ADA News http://r.smartbrief.com/resp/nWivCJwxjADnukhiCifOisBWcNCrkw?format=multipart> (5/24)
Source: https://jada.ada.org/
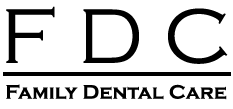
Wisconsin has the best oral health in the United States and Mississippi has the worst, according to WalletHub and its latest annual report of States with the Best & Worst Dental Health, based on 26 key metrics.
Criteria included the percentage of adolescents who visited a dentist in the past year, treatment costs, life satisfaction due to oral conditions, dentists per capita, sugar-sweetened beverage consumption, percentage of smokers, and other factors.
WalletHub used data from the Census Bureau, the Bureau of Labor Statistics, the Centers for Disease Control and Prevention, the Center for Health Care Strategies, the ADA, the Health Resources & Services Administration, and other stakeholders.
Wisconsin topped the list for the third year in a row, followed by Illinois, the District of Columbia, Minnesota, Connecticut, North Dakota, Michigan, Idaho, Massachusetts, and New Jersey rounding out the top 10.
Mississippi had the worst oral health for the second year in a row, and it was preceded in the bottom 10 by West Virginia, Arkansas, Montana, Louisiana, Alabama, Texas, Alaska, Florida, and California.
In other findings:
- Rhode Island has the lowest share of the population who couldn’t afford more dental visits due to costs, 37%, which was half of what Georgia reported at 74%.
- The District of Columbia has the most dentists per 100,000 residents, 68, which is 3.4 times more than Louisiana, which had the fewest at 20.
- The District of Columbia has the highest share of the population receiving fluoridated water, 100%, while Hawaii had the lowest share at 8.8%.
- Minnesota, Hawaii, and Illinois have the lowest share of adults with poor or fair oral condition, 22%, while Montana had the highest at 40%.
Noting that February is National Children’s Dental Health Month, WalletHub also noted how shaping positive oral health behaviors among children can lead to better oral health in adulthood.
“Beyond brushing and flossing, it is important to instill the value of good oral hygiene in people from a young age,” said FazianKabani, PhD, MBA, MHA, RDH, assistant director for diversity and faculty development and assistant professor at the Texas A&M College of Dentistry.
“Multiple theories suggest that people act upon health behaviors when they understand and are motivated by a particular value system. Therefore, it is imperative to teach children the value of good dental hygiene to yield a better prospect of good oral health as they grow and develop,” Kabani said.
Public health programs such as community water fluoridation and school sealant programs can have a positive impact on oral health as well, WalletHub said.
“Evidence has shown community water fluoridation to be an effective intervention for reducing the presence of dental caries in communities. It is important to note that a regulated dose of fluoride, 0.7 ppm, has been established for effective community water fluoridation,” said Kabani.
Kabani also noted that evidence continues to demonstrate the effectiveness of sealants in preventing tooth decay on the occlusal surfaces of teeth.
“Statistics demonstrate that health disparities are found more among lower-income, minority, and immigrant populations. Indeed, school sealant programs should be extended more aggressively, particularly in lower-income areas, to better prevent dental caries in children, but should also be extended to areas the contain diverse populations,” he said.
WalletHub further noted the impact that costs can have on people pursuing dental treatment, however, though public health may be able to help there as well.
“Oral healthcare can become more affordable through changes in public health policy and practice, most notably via allocating more public health funds towards oral healthcare services,” Kabani said.
“Unfortunately, people have to purchase a separate dental health insurance plan, because oral healthcare is not typically a covered service under general health insurance. We need to advocate for changes in public health policy to bridge the gap between medical and dental to help ensure a more affordable experience for the public,” he said.
“Fortunately, pediatric dental care is considered an essential healthcare service under the reformed national healthcare policy. However, adult and geriatric dental care remain an uncovered service, albeit for certain circumstances,” Kabani said.
“Medicaid and Medicare should both provide coverage for oral healthcare services, particularly because these government programs are intended to provide support to some of society’s most vulnerable populations,” he said.
Source: Dentistry Today
We recently purchased 2 Extraoral Suction Technology units!
What is an Extraoral Suction Technology unit?
Extraoral suction units remove 99.9% of aerosolized droplets of saliva, blood, and other fluids that can be emitted from a patient’s mouth during routine dental treatment.
How Extraoral Suction Works
During treatment, doctors and hygienists utilize ultrasonic scalers, syringes, and high-speed and low-speed handpieces, all of which generate a large amount of water and mist, which, combined with saliva, blood, and other tissue, produce aerosols.
The extraoral suction device, which resembles the end of a vacuum cleaner with a clear funnel-shaped attachment positioned just outside the mouth, removes these aerosols to prevent them from passing between doctors and patients.
With strong suction vacuum pressure and a high air-suction flow rate, the aerosol droplets between the doctor or staff member and the patient are sucked into the machine through the adjustable positioning arm.
The aerosol is then decontaminated as it goes through a four-stage filtration and disinfection process, including an initial HEPA filter, ultraviolet-C light chamber, plasma generator, and large HEPA-13 filter. Ultimately, the droplets are discharged from the machine after thorough purification.
Having the extraoral suction unit in place keeps dental appointments efficient, reduces the risk of splatter, and allows dental hygienists to use the ultrasonic scaler in addition to hand scaling, resulting in better stain and tartar removal—and tartar is the direct cause of periodontal disease and bad breath.
Source: Dentistry Today
Aging and Dental Health

- The demographic of older adults (i.e., 65 years of age and older) is growing and likely will be an increasingly large part of dental practice in the coming years.
- Although better than in years past, the typical aging patient’s baseline health state can be complicated by comorbid conditions (e.g., hypertension, diabetes mellitus) and physiologic changes associated with aging.
- Older adults may regularly use several prescription and/or over-the-counter medications, making them more vulnerable to medication errors, drug interactions or adverse drug reactions.
- Potential physical, sensory, and cognitive impairments associated with aging may make home oral health care and patient education/communications challenging.
- Dental conditions associated with aging include dry mouth (xerostomia), root and coronal caries, and periodontitis; patients may show increased sensitivity to drugs used in dentistry, including local anesthetics and analgesics.
The Federal Interagency Forum on Aging-Related Statistics projects that by the year 2030, the number of U.S. adults 65 years or older will reach 72 million, representing nearly 20% of the total U.S. population; this is an approximate doubling in number as compared to the year 2000. Older adults are, therefore, a growing patient demographic for dental practices. Although around 5% of adults older than 65 years are edentulous, increased numbers of older adults are retaining their natural teeth compared with previous cohorts. According to a 1999-2004 National Health and Nutrition Examination Survey (NHANES), approximately 18% of adults aged 65 years or older with retained natural teeth have untreated caries while a 2009-2012 NHANES found that 68% of these patients have periodontitis. Consideration of the overall clinical and oral health context of aging patients is important in order to provide optimum dental care.
For more information visit https://www.ada.org/en/member-center/oral-health-topics/aging-and-dental-health
Content on the Oral Health Topics section of ADA.org is for informational purposes only. Content is neither intended to nor does it establish a standard of care or the official policy or position of the ADA; and is not a substitute for professional judgment, advice, diagnosis, or treatment. ADA is not responsible for information on external websites linked to this website.
Pandemic-Related Stress May Be Affecting Oral Health
Noting that “reports of a huge spike in cracked teeth have received national media attention in recent days,” USA Today (9/11, Shannon) said some dentists say they are seeing signs the coronavirus pandemic may be affecting oral health in additional ways, with some observing that they are treating more patients with inflamed gums and in need of treatment than before the pandemic. Part of the reason for an upward trend in oral health problems may stem from the pandemic’s “ripple effect – another example of how the pandemic has altered daily lives and led to unexpected health problems.” Before the pandemic, “your day had a rhythm to it,” Dr. Matthew Messina, a spokesperson for the ADA, told USA TODAY. When that rhythm is interrupted, it can be easy to forget “simple little things like oral hygiene.” Another reason may stem from patients delaying dental visits due to concerns about the coronavirus. “While they can’t eliminate all risk, dentists across the nation are taking steps to minimize the chances of spreading the coronavirus,” the article said.
Concerning the uptick in fractured teeth that some dentists are observing amid the pandemic, Inside Edition (9/13) spoke with a dentist who “said the key is to reduce stress that causes the clenching and grinding, and one way to do is through exercise.” Wearing a mouth guard at night can also protect teeth, the dentist said.
Writing in the Washington Post (9/11), journalist Emily Sohn shared her experience with a cracked tooth and filling, noting her dentist “says she has seen a surge in problems related to tooth-grinding and jaw-clenching” since the pandemic began. Sohn shared information on the potential causes of bruxism and some possible solutions.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for additional information on bruxism. In addition, the ADA Catalog offers the book Understanding Bruxism: Current Knowledge and Practice.
Dental Visits Listed Among Appointments People Should Prioritize Right Now
In a consumer-focused article, U.S. News & World Report (9/9, Howley) said, “The coronavirus pandemic that took hold this past spring upended normal life for just about everyone, and for many people, that meant delaying health care appointments.” Now that more is known about the virus and how it is transmitted and access to personal protective equipment has improved, the article stated that “health care providers from across the whole health care spectrum are urging patients to reschedule appointments that may have been canceled or postponed.” With this in mind, the article said “any routine appointment that has been put off should be rescheduled as soon as possible,” and dental visits are among “appointments that might take priority.”
Dental Care Is Rebounding
Axios (8/17, Herman) reported dentists’ offices “are reopening and working overtime, and dental suppliers are optimistic things are close to returning to normal after the coronavirus put the industry on ice for almost two months.”
The Bakersfield (CA) Californian (8/19, Cox, Subscription Publication) reports that dentists “are trying to clear up confusion about cautionary guidance issued earlier this month by the World Health Organization.” WHO’s “missive, reported by news organizations across the United States, advised delaying non-essential dental care – but only in places where community transmission of COVID-19 is elevated or at the recommendation of local, regional or national officials.” ADA President Chad P. Gehani said in a statement in response to the guidance, “Oral health is integral to overall health. Dentistry is essential health care. … Dentistry is essential health care because of its role in evaluating, diagnosing, preventing or treating oral diseases, which can affect systemic health.” Meanwhile, WHO’s chief dental officer, Benoit Varenne, “felt obliged to issue a statement Aug. 13 saying news media headlines ‘intentionally or not’ failed to mention the organization’s guidelines ‘is only suggested in an intense uncontrolled community transmission scenario.’”
The Pittsburgh Tribune-Review (8/19, Guggenheimer) reports Varonne said, “In our guidance, WHO advises that routine non-emergency care be delayed until there has been a significant reduction in covid-19 transmission rates … Unfortunately, a number of media headlines, intentionally or not, did not mention that the recommendation to delay routine oral health care is only suggested in an intense uncontrolled transmission scenario, a scenario that does not fit with the current situation of most countries around the world.”
HealthDay News (8/19) reports the ADA and the CDC have “called on dentists to use personal protective equipment, such as masks, goggles and face shields.” Gehani is quoted saying, “Millions of patients have safely visited their dentists in the past few months for the full range of dental services. … With appropriate PPE, dental care should continue to be delivered during global pandemics or other disaster situations.”
To access the ADA’s Return to Work Interim Guidance toolkit, which recommends measures to take to help protect patients, staff and dentists from COVID-19 as dental practices re-engage in providing the full range of oral health care, visit ADA.org/returntowork.
Information for the public on what to expect as dental offices reopen may be found on ADA’s consumer website MouthHealthy.org, and The Journal of the American Dental Association has a “For the Patient” page, Protecting You During Your Dental Visit.
Dentists Should Be Offered Early Access To SARS-CoV-2 Vaccine, ADA Says
The ADA News (9/4, Burger) reported, “Dentists are essential health care workers who should be afforded early access to a safe and effective SARS-CoV-2 vaccine when one becomes available, ADA Executive Director Kathleen T. O’Loughlin told a National Academies of Sciences, Engineering, and Medicine panel Sept. 2.” The panel is working on “a plan for equitable distribution of the vaccine.” In her remarks, Dr. O’Loughlin “noted that 15% of the American public did not feel comfortable visiting the dentist without a medical breakthrough, according to a poll.” She said, “Early access to a safe and effective SARS-CoV-2 vaccine will reassure this group of patients that it is safe to resume dental appointments and will furthermore reassure dental health care practitioners who have reservations about delivery of dental care.” Dr. O’Loughlin and ADA President Chad P. Gehani also sent “a Sept. 4 letter to the National Academies affirming that dentists should be included among those who have early access to a vaccine when available.”
For more information about the ADA’s advocacy efforts during COVID-19, visit ADA.org/COVID19Advocacy .
Evidence Does Not Support Classifying Fluoride As Cognitive Neurodevelopmental Hazard, Review Finds
The ADA News (3/10, Burger) reports, “The National Academies of Sciences, Engineering, and Medicine announced March 5 that it does not find that the National Toxicology Program adequately supported its conclusion that fluoride is ‘presumed’ to be a cognitive neurodevelopmental hazard to humans.” The academies’ review of the National Toxicology Program’s draft monograph comes “after months of concern and anticipation from all who are invested in the developing science around water fluoridation.” After the review was released, the ADA’s National Fluoridation Committee issued a statement: “Based on the major concerns raised by the National Academies of Sciences, Engineering, and Medicine review, it is hoped that the National Toxicology Program will substantially revise their draft monograph and provide an adjusted statement to better reflect the status of current science with respect to the cognitive neurodevelopmental hazard of fluoride to humans.”
The ADA-published reference “Fluoridation Facts” is available to view or download at no cost. Additional free ADA resources on community water fluoridation are located online at ADA.org/fluoride.
Dental professionals can point their patients to the ADA’s consumer website, MouthHealthy.org/fluoride, for more information. In addition, The Journal of the American Dental Association offers the patient handout Drink Up! Fluoridated Water Helps Fight Decay, and the ADA Catalog features the Fluoride: Nature’s Cavity Fighter brochure.
Periodontal Disease May Increase Risk For Age-Related Macular Degeneration, Review Suggests

Healio (2/13, McGee) reported that periodontal disease (PD) may increase the risk for age-related macular degeneration (AMD), according to a literature review published in The Permanente Journal, although “the link between the two is still unclear.” The article added that “PD and AMD share similar risk factors such as inflammation disorders, advanced age, smoking habits and diabetes, said the authors,” and additional studies are needed to better understand the relationship between the two.
Dental professionals can find additional information on oral-systemic health on an ADA Science Institute-developed Oral Health Topics page.
Kombucha, Gummy Vitamins Among Trending Foods That May Harm Teeth

In a consumer-focused article, Real Simple (1/23, Gold) said that “some of the most popular health foods today” may actually harm teeth. For instance, kombucha has become “a huge health trend over the past few years,” but the fermented tea drink’s acidity could be problematic. The article explained that kombucha has a low pH value, which could lead to dental erosion. Another “rising trend” is “the consumption of gummy vitamins that claim to lead to thicker hair, nails, improved sleep, higher energy, and more.” Chewing these products can leave a “sticky sugar residue” on teeth, increasing the risk of tooth decay. In addition, the article discussed how hard seltzers, pumpkin spice lattes, mulled wine, and turmeric may also negatively affect teeth.
The Oral Health Topics on ADA.org provide additional information on erosive tooth wear and nutrition and oral health for dental professionals.
The ADA Catalog features the brochure Snack And Sip All Day? Risk Decay!
Study: Decreased Tongue Fat May Help Reduce Severity Of Sleep Apnea

The Inquirer (PA) (1/10, McCullough) reported that “weight loss has been shown to reduce or even cure sleep apnea in people who are overweight,” and a recent “study led by University of Pennsylvania researchers suggests the main reason is that dropping pounds causes the tongue to shrink, mostly by losing fat.” The findings were published in the American Journal of Respiratory and Critical Care Medicine.
Newsweek (1/10, Gander) reported the study included “67 obese people aged 49 on average with obstructive sleep apnea.” Researchers “found weight loss decreased tongue fat, and that in turn appeared to reduced the severity of sleep apnea.”
Dental professionals can point their patients to the ADA’s consumer website, MouthHealthy.org, for information about sleep apnea.
Acupuncture May Ease Dry Mouth Symptoms Associated With Radiation Therapy, Research Suggests

HealthDay (12/27, Reinberg) reported that “dry mouth can be a troubling side effect of radiation therapy,” but a new study suggests “acupuncture may ease its symptoms.” Among 339 patients receiving radiation treatment for cancer, researchers found that “those who had acupuncture had fewer symptoms of dry mouth (xerostomia) than those who didn’t have acupuncture.” Specifically, “a year after treatment, 35% of acupuncture patients had dry mouth, compared to 48% of those given fake acupuncture and 55% of those who didn’t get acupuncture, the findings showed.” The study was published in JAMA Network Open.
The Oral Health Topics on ADA.org and MouthHealthy.org provide information on xerostomia for dental professionals and for patients.
Biotene Dry Mouth Oral Rinse has become the first product to earn the ADA Seal of Acceptance in the dry mouth product category. To learn more about the Seal program, go to ADA.org/Seal.
Cell Phone Injuries To Face Have Risen Sharply Over Past 20 Years
 The AP (12/5, Tanner) reported researchers have found “a spike” in US emergency department (ED) treatment for “facial cuts, bruises and fractures” due to cellphones. For the study, investigators examined 20 years of ED data, finding “an increase in cellphone injuries starting after 2006, around the time when the first smartphones were introduced.” While “some injuries were caused by phones themselves, including people getting hit by a thrown phone,” the study also found that “many were caused by distracted use including texting while walking, tripping and landing face-down on the sidewalk.”
The AP (12/5, Tanner) reported researchers have found “a spike” in US emergency department (ED) treatment for “facial cuts, bruises and fractures” due to cellphones. For the study, investigators examined 20 years of ED data, finding “an increase in cellphone injuries starting after 2006, around the time when the first smartphones were introduced.” While “some injuries were caused by phones themselves, including people getting hit by a thrown phone,” the study also found that “many were caused by distracted use including texting while walking, tripping and landing face-down on the sidewalk.”
According to CNN (12/5, LaMotte), the study revealed that “most injuries occurred to people between the ages of 13 and 29 and were due to distracted driving, walking and texting with a cell phone.” Researchers also “found injuries to children 13 and younger were more likely to be due to direct mechanical injury from the cell phone.” The findings were published online in the journal JAMA Otolaryngology-Head & Neck Surgery.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for information on dental emergencies.
Ohio State Study Finds Oral Health, Diet May Improve Psoriasis
 A new study by researchers at The Ohio State University Wexner Medical Center is giving insight into certain lifestyle choices that may prevent or improve psoriasis, helping experts better understand what triggers the disease.
A new study by researchers at The Ohio State University Wexner Medical Center is giving insight into certain lifestyle choices that may prevent or improve psoriasis, helping experts better understand what triggers the disease.
Dental health and diet may have an impact on the development and severity of psoriasis, according to a study by dermatologists at The Ohio State University Wexner Medical Center. Psoriasis is a skin disease that causes thick, itchy patches of red skin with silvery scales and affects more than 8 million Americans.
The study found psoriasis patients who rated their gum health as poor or very poor exhibited significantly more severe psoriasis symptoms than those with healthy gums. Conversely, patients who reported consuming fresh fruit at least once a day experienced milder psoriasis symptoms. The study was published in the Dermatology Online Journal.
“Psoriasis is an autoimmune disease so although it often presents as red, scaly patches on the skin, we know that the causes and consequences are more than skin deep,” said Dr. Benjamin Kaffenberger, a dermatologist at the Ohio State Wexner Medical Center who led the study.
Psoriasis, which can last a lifetime, is caused by a problem with the immune system. In a process called cell turnover, skin cells that grow deep in the skin rise to the surface. Normally this takes a month but with psoriasis, it happens in just a few days because the cells rise too quickly. Treatments include creams, medicines and ultraviolet light therapy.
“We’re looking for some sort of trigger that sets off the immune system. Because strep throat is one of the known triggers and the microbiome of bacteria in the mouth is much more complex, that became our starting point,” said Kaffenberger, who is also an associate professor in Ohio State’s College of Medicine. “We wondered if poor dental health could be a risk factor for psoriasis.”
Researchers created a specially designed lifestyle and diet questionnaire that was administered to 265 patients at Ohio State’s dermatology clinics. The study surveyed 100 patients with psoriasis and 165 without the disease. The study showed poor dental and oral health, in particular gum pain, was associated with those who had psoriasis.
“Patients who had more severe psoriasis were more likely to report that their gums were in worse condition than patients who didn’t have mild to moderate psoriasis in the first place,” Kaffenberger said. “And patients who had higher fruit consumption reported less significant psoriasis, indicating fruit and potentially fresh foods may be an associated protective factor.”
The study also reinforced data from previous studies that found family history of psoriasis, smoking and obesity were significant predictors of psoriasis.
Kaffenberger hopes to expand the study outside Ohio State’s dermatology clinics and survey thousands of psoriasis patients with varying degrees of the disease. While Kaffenberger noted that the study’s results were very preliminary, he believes having dermatologists screen for dental health and counsel psoriasis patients for improved dietary health may help them.
“Psoriasis is a chronic disease and can be so severe that it covers the entire body. Patients ask us ‘If I change my diet, will I get rid of this disease?’ That’s what really drove the onset of this study – to see what health and lifestyle changes patients could make,” Kaffenberger said. “The key is to protect your gums and your mouth by brushing your teeth twice a day and flossing. Lifestyle changes include quitting smoking, avoiding high alcohol consumption and properly managing diabetes.”
Study Finds Sugary Drinks Associated With Dental Erosion, Obesity

UPI (10/28, Dunleavy) reports a new study published in the journal Clinical Oral Investigations suggests that dental erosion and obesity may have “at least one common link – sugar-sweetened beverages.” After analyzing “data from 3,541 American adults,” with about two thirds “either overweight or obese, based on body mass index,” researchers from King’s College London found that “overall, more than 12 percent of the adults studied had moderate to severe tooth wear, with an average of 3.4 tooth surfaces affected.” In adults “who regularly drank soda and other soft drinks, the number of teeth affected by wear was 1.4 times higher per sugary beverage consumed per day.”
International Business Times (10/29, Mathew) reports, “The research team concluded the study by stating that consumption of sugar-sweetened acidic drinks is a common cause of both obesity and tooth decay.”
In a release picked up by News Medical (10/28), lead author Dr. Saoirse O’Toole from King’s College London said, “This is an important message for obese patients who are consuming calories through acidic sugar sweetened drinks. These drinks may be doing damage to their body and their teeth.”
Dr Bicuspid (10/28, Busch) also reports.The Oral Health Topics on ADA.org provide additional information on erosive tooth wear and nutrition and oral health for dental professionals.
Former Nationals Outfielder Turned Dental Student Analyzes World Series

The ADA News (10/24, Garvin) reports that fans of the Washington Nationals tuning into Fox-5 DC (WTTG-TV) for the World Series “might see a familiar face smiling back at them: Former Nationals outfielder Justin Maxwell, who is a part of the station’s broadcast team.” The article explains that Mr. Maxwell is now “a second-year dental student at the University of Maryland School of Dentistry,” but he “has always enjoyed the idea of broadcasting.” When WTTG-5 began “putting together its own World Series team, they reached out to him to see if he’d be interested. He was.” The article notes that Mr. Maxwell played “professional baseball for more than 10 years,” before deciding in 2016 to focus on becoming a dentist. When asked if he would consider leaving dental school to pursue broadcasting full time, Mr. Maxwell said, “Absolutely not. No way!”
Editor’s note: The World Series resumes Friday, Oct. 25, at 8 p.m., nationally, on Fox. Readers living in the Washington viewing area can catch Maxwell during Fox-5’s 5:30 p.m. newscasts and 6:30 p.m. pregame shows Oct. 25-27.
No Scientific Evidence Brushing With Table Salt Whitens Teeth, ADA Spokesperson Says

CNN (10/3, Drayer) states that people should avoid using table salt to whiten teeth. “I see no clinical reason why someone would brush their teeth with salt,” said Dr. Matt Messina, an American Dental Association spokesperson. “There is no scientific evidence that brushing with salt has any sort of whitening effect on teeth.” In addition, since salt is abrasive, using it on teeth could damage enamel. Instead, regularly brushing teeth with a toothpaste with the ADA Seal of Acceptance and cleaning between teeth can help whiten teeth. For those considering teeth whitening, Dr. Messina encourages consulting with a dentist. “There are safe and effective whitening techniques, but they will be different for each individual person,” he said.
Dental professionals can find additional information on whitening on an ADA Science Institute-developed Oral Health Topics page. The ADA also offers the brochure Tooth Whitening for a Better Smile.
Dental professionals can direct their patients to MouthHealthy.org, ADA’s consumer website, for evidence-based information about teeth whitening. The ADA also provides a complete list of bleaching products with the ADA Seal of Acceptance.
Gum Disease May Increase Hypertension Risk, Review Suggests

The New York Times (9/25, Bakalar) reports that “people with gum disease may be at increased risk for high blood pressure,” researchers concluded after analyzing “the results of 81 studies including more than 200,000 people.” The findings were published in Cardiovascular Research, a journal of the European Society of Cardiology.
The Atlanta Journal-Constitution (9/24, Parker) reports that the researchers from University College London found “moderate-to-severe periodontitis was linked with a 22% higher hypertension risk, while severe periodontitis was linked with 49% higher risk.”
In a release on Science Daily (9/24), senior author Dr. Francesco D’Aiuto said, “We observed a linear association – the more severe periodontitis is, the higher the probability of hypertension.”
Dental professionals can point their patients to the ADA’s consumer website, MouthHealthy.org, for additional information on periodontitis. The ADA Catalog also offers the brochure Periodontal Disease: Your Complete Guide.
Children Under Age Five Should Drink Mostly Milk And Water, New Guidelines Say

The New York Times (9/18, Rabin) reports that on Sept. 18, “a panel of scientists issued new nutritional guidelines for children…describing in detail what they should be allowed to drink in the first years of life.” The guidelines recommend that “for the first five years, children should drink mostly milk and water.”
CNN (9/18, Christensen) reports, “Most children under the age of five should avoid plant-based milk, according to new health guidelines about what young children should drink” and issued by “a panel of experts with the Academy of Nutrition and Dietetics, the American Academy of Pediatric Dentistry, the American Academy of Pediatrics and the American Heart Association.” With the exception of soy milk that has been fortified, “plant-based milk made from rice, coconut, oats or other blends…lack key nutrition for early development, according to [the] guidelines.” In addition, “they should also avoid diet drinks, flavored milks and sugary beverages and limit how much juice they drink, the guidelines said.”
Information about the ADA’s nutrition-related activities is available at ADA.org/nutrition.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for up-to-date and evidenced-based information about nutrition. The ADA Catalog also features the brochure Sip and Snack All Day? Risk Decay!
Vitamin D Intake During Pregnancy Linked to Child’s Enamel Defects

Children born to women who received high doses of vitamin D during pregnancy had a 50% lower risk of enamel defects in permanent dentition than those whose mothers received a standard dose, according to a report in JAMA Pediatrics. Findings from the study, “Association of High-Dose Vitamin D Supplementation During Pregnancy With the Risk of Enamel Defects in Offspring,” imply prenatal vitamin D supplementation may serve as a preventive intervention for enamel defects
Many Americans Unaware Of Cancers Associated With HPV, Survey Suggests
 NBC News (9/16, Edwards) reports a study of over 6,000 men and women indicates “the majority of American adults are unaware” that “HPV, or human papillomavirus, can lead to a variety of cancers,” including oropharyngeal cancer. The survey found that while “two-thirds of women 18 to 26 understood that HPV can cause cervical cancer,” only one-third of men in that age bracket knew about the connection between HPV and cervical cancer. Moreover, “overall, 70 percent of adults of any age were unaware of the link between HPV and other cancers.” The findings were published in JAMA Pediatrics.
NBC News (9/16, Edwards) reports a study of over 6,000 men and women indicates “the majority of American adults are unaware” that “HPV, or human papillomavirus, can lead to a variety of cancers,” including oropharyngeal cancer. The survey found that while “two-thirds of women 18 to 26 understood that HPV can cause cervical cancer,” only one-third of men in that age bracket knew about the connection between HPV and cervical cancer. Moreover, “overall, 70 percent of adults of any age were unaware of the link between HPV and other cancers.” The findings were published in JAMA Pediatrics.
HealthDay (9/16, Reinberg) reports, “The researchers found that among people eligible for the vaccine, only 19% of men and 31.5% of women had been advised” by their health provider to get vaccinated against HPV. “The message from providers can be as simple as: ‘I strongly believe in the importance of this cancer-preventing vaccine for [your child],’” said Dr. David Fagan, vice chair of pediatrics at Cohen Children’s Medical Center in New Hyde Park, New York. “I find it effective to emphasize the parents’ role in preventing their child from getting HPV-related cancers.”
An ADA Science Institute-developed Oral Health Topics page on cancer (head and neck) offers information on HPV, detection, ADA policies, and resources for dentists. The National HPV Vaccination Roundtable guide for dental healthcare providers also offers information on how dental professionals “play a critical role in combating growing rates of HPV-positive oropharyngeal cancers.”
ADA CE Online offers the course HPV Infection, Risk Factors, and HPV-Related Oropharyngeal Cancer. In addition, the ADA Catalog offers the Oral Health and the HPV Vaccine brochure.
On Sept. 25, from noon to 1 PM Central time, the ADA Council on Advocacy for Access and Prevention will present the webinar, “Say What? Science and Skills for Taking About the HPV Vaccine.” Register online or read more about it at ADA News.
Dentists can refer patients to MouthHealthy.org for information on oral cancer and HPV and oropharyngeal cancer, and JADA For the Patient also includes the article Vaccines for your child.
Consumption Of Soft Drinks May Raise Risk Of Premature Death, Research Suggests
 Newsweek (9/3, Gander) reports a study published in JAMA Internal Medicine suggests “both sugary and diet soft drinks” are associated with “an increased risk of death.” The research, which involved over 450,000 people from 10 European countries, found “participants who drank a lot of soft drinks were at a greater risk of death by any cause compared with those who drank the lowest amounts.”
Newsweek (9/3, Gander) reports a study published in JAMA Internal Medicine suggests “both sugary and diet soft drinks” are associated with “an increased risk of death.” The research, which involved over 450,000 people from 10 European countries, found “participants who drank a lot of soft drinks were at a greater risk of death by any cause compared with those who drank the lowest amounts.”
CNN (9/3, Lamotte) reports the study “found those who drank two or more glasses of any type of soda a day had a higher risk of dying from any cause of death than people who drank less than a glass each month.” Furthermore, the investigators “found men and women who drank two or more glasses a day of sugar-sweetened soft drinks had a higher risk of dying from digestive disorders, while those who drank the same amount of diet drinks had higher risks of dying from cardiovascular disease.”
HealthDay (9/3, Gordon) says while the study found an association, it “does not prove a cause-and-effect relationship between soda and a higher risk of early death.”
Information about the ADA’s nutrition-related activities is available at ADA.org/nutrition.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for up-to-date and evidenced-based information about nutrition. The ADA Catalog also features the brochure Sip and Snack All Day? Risk Decay!
Vaping Can Have Similar Effect On Teeth As Cigarette Smoking, ADA Spokesperson Says

Health (8/27, O’Neill) discusses the effects vaping may have on the teeth, featuring information from American Dental Association spokesperson Dr. Matthew Messina. Vaping adds “heat in the mouth,” Dr. Messina says, which “changes the bacterial presence in the mouth. It dries the mouth out.” Dr. Messina adds, “[The] rate of tooth decay increases, sometimes dramatically, if we dry the mouth out.” In addition, vaping can lead to tooth discoloration because of the presence of nicotine, inflamed gum tissue, and bone loss, he says. “It’s important to stress the fact that while vaping is new and is being actively studied, we have to consider vaping and cigarette smoking relatively the same, as far as the effects on the teeth and gum tissues,” says Dr. Messina.
Last week, the New York Times (8/23, Richtel, Kaplan) reported that public health officials announced the first vaping-related death. In a media statement, the Centers for Disease Control and Prevention said the “death in Illinois reinforces the serious risks associated with e-cigarette products.”
Follow the ADA’s advocacy efforts on tobacco at ADA.org/tobacco.
Prenatal Vitamin D Intake May Reduce Risk Of Enamel Defects In Children, Study Suggests

The New York Times (8/13, Bakalar) reports, “Women who take large doses of vitamin D during pregnancy may be giving their children a lower risk of dental problems,” a “double-blinded clinical trial” suggests. Researchers randomly assigned 623 women into two groups and beginning on the “24th week of pregnancy, one group took two pills daily, one containing 400 units and the other 2,400 units of vitamin D,” while the other “took a 400 unit pill plus an identical-looking placebo.” Researchers “found that children of women who took the vitamin D regimen had a 47 percent lower rate of enamel defects in both permanent and baby teeth than those in the control group.” The study was published in JAMA Pediatrics.
The course Mouthful of Lesions in Peewees: Maximizing Infant Oral Health will be offered at the ADA FDI World Dental Congress, held in San Francisco Sept. 4-8.
Information about the ADA’s nutrition-related activities is available at ADA.org/nutrition.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for up-to-date and evidenced-based information about nutrition.
Zip Code May Be Key Factor In Predicting Lifespan, Evidence Suggests

TIME (6/17, Ducharme, Wolfson) reports that a “growing body of evidence suggests it may be a person’s zip code that holds the most information about how long they’ll live.” Researchers from the New York University School of Medicine examined data from “NYU Langone Health’s City Health Dashboard,” finding that “56 of the U.S.’ 500 largest cities are home to people who can expect to live at least 20 fewer years than those in other neighborhoods.” The article says that “a zip code’s influence on the health of those living there is multifold,” explaining that where a person lives directly affects their health “in a number of ways, from exposure to air pollution and toxins to accessibility of healthy food, green space and medical care,” and it is also “a more subtle indicator of socioeconomic factors that are inherent to health and longevity, including race and income.”
Kombucha May Harm Enamel

Vice (7/29, Castrodale) discusses how kombucha may harm teeth, sharing comments from several dentists who explain that the fermented tea drink’s acidity could contribute to dental erosion. The article notes that the American Dental Association shared an article on kombucha on its Facebook page. For those who consume kombucha, the article reports that some dentists suggest “limiting yourself to versions that are lower in sugar, downing it all in one sitting (to minimize the amount of time that your mouth pH is altered), drinking it through a straw, and rinsing your mouth out with water after you finish the bottle.” The article adds that people could also choose to “stick with water.”The Oral Health Topics on ADA.org provides additional information on dental erosion for dental professionals.
The ADA Catalog features the brochures, Tooth Erosion: The Harmful Effects of Acid and Snack And Sip All Day? Risk Decay!
In addition, Crest Pro-Health Advanced Deep Clean Mint Toothpaste is the first ADA Seal product in the enamel erosion control category.
Future Retirees Often Overlook Dental Care Costs
 Business Insider (5/2, Loudenback) reported that although data indicate “over a third of US adults are more concerned about covering health costs in retirement than paying off debt and affording lifestyle expenses right now,” only “about half have a financial plan in place for the future.” In addition, Business Insider stated that dental care costs are among some of “the most overlooked health costs in retirement.”
Business Insider (5/2, Loudenback) reported that although data indicate “over a third of US adults are more concerned about covering health costs in retirement than paying off debt and affording lifestyle expenses right now,” only “about half have a financial plan in place for the future.” In addition, Business Insider stated that dental care costs are among some of “the most overlooked health costs in retirement.”
The Motley Fool (5/3, Backman) added, “That said, 75% of people with a health savings account, or HSA, do have a plan for covering future medical costs.” The article discussed HSAs, noting they can be used to pay for “common medical expenses,” including dental care.
The Oral Health Topics on ADA.org and MouthHealthy.org provide information on aging and dental health for dental professionals and patients.
Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for a guide to finding and paying for dental care.
Many US Adults Unfamiliar With Key Dental Terms, Survey Finds
 In a release on PRNewswire (5/15), Delta Dental Plans Association states its “new Adult’s Oral Health & Well-Being Survey indicates that a significant portion of the American population is not familiar with certain key dental terms.” The survey of 1,100 adults in the US found “that the majority of adults are not versed in bruxism (81%), caries (75%) and prophylaxis (64%).” In addition, the survey found that 33% are unfamiliar with what periodontal disease is, and 40% are unsure what the term sealant means.
In a release on PRNewswire (5/15), Delta Dental Plans Association states its “new Adult’s Oral Health & Well-Being Survey indicates that a significant portion of the American population is not familiar with certain key dental terms.” The survey of 1,100 adults in the US found “that the majority of adults are not versed in bruxism (81%), caries (75%) and prophylaxis (64%).” In addition, the survey found that 33% are unfamiliar with what periodontal disease is, and 40% are unsure what the term sealant means.
Excessive Consumption Of Sugary Beverages May Shorten Life, Research Suggests

CNN (5/17, Scutti) reported that “a study links drinking too many sugary beverages – and even 100% natural fruit juices – to an increased risk of early death.” CNN said the study, which was published in JAMA Network Open, found that “people who consumed 10% or more of their daily calories as sugary beverages had a 44% greater risk of dying due to coronary heart disease and a 14% greater risk of an early death from any cause compared with people who consumed less than 5% of their daily calories as sugary beverages.” While the study had several limitations, including that sugary drink consumption was based on self-reporting, co-author Dr. Jean A. Welsh, an assistant professor at Emory University in Atlanta, said, “Sugary beverages, whether soft drinks or fruit juices, should be limited.”
Information about the ADA’s nutrition-related activities is available at ADA.org/nutrition. Dentists can refer patients to MouthHealthy.org, ADA’s consumer website, for up-to-date and evidenced-based information about nutrition.
Studies Find Association Between Oral Health, Systemic Health

The New York Post (6/4, Sparks) reports on recent studies that have found an association between poor oral health and Alzheimer’s disease, ischemic stroke, and high blood pressure, among other health issues. For instance, the article reports a study by researchers in Norway found Porphyromonas gingivalis may play a role in the development of Alzheimer’s disease. In another study, researchers were “able to pinpoint common oral pathogens in 79% of cerebral blood clots samples of 75 stroke patients.” A related 2018 study also found an association between high blood pressure and poor oral health, and Dr. Davide Pietropaoli, the study’s lead investigator, said, “Oral health is indispensable to overall physiological health.”
Poor Oral Health Associated With Increased Liver Cancer Risk, Study Suggests

Medical Xpress (6/17) states that researchers at Queen’s University Belfast “investigated the association between oral health conditions and the risk of a number of gastrointestinal cancers, including liver, colon, rectum and pancreatic cancer.” The release states that although “no significant associations were observed on the risk of the majority gastrointestinal cancers and poor oral health, a substantial link was found for hepatobiliary cancer.” The findings were published in the United European Gastroenterology Journal.